Home » Endoscopic Spine Surgery
GET OFFER
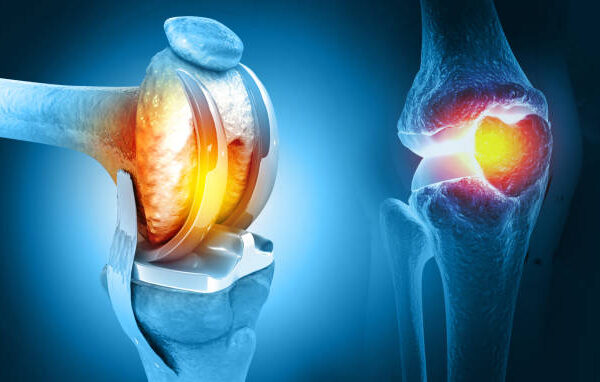
Endoscopic Spine Surgery (ESS) is a minimally invasive surgical technique used to treat various spine-related conditions. This approach utilizes a small endoscope and specialized instruments to access and treat spinal structures with minimal disruption to surrounding tissues. ESS is gaining popularity due to its ability to reduce recovery times, minimize scarring, and lower the risk of complications compared to traditional open spine surgery.
Indications for Endoscopic Spine Surgery
ESS is suitable for treating a variety of spine conditions, including:
- Herniated Disc: Removal of disc material causing nerve compression.
- Spinal Stenosis: Widening of the spinal canal to alleviate pressure on nerves.
- Degenerative Disc Disease: Treating damaged discs to reduce pain and improve mobility.
- Sciatica: Relieving nerve compression to address radiating leg pain.
- Spinal Instability: Repairing structures to stabilize the spine.
- Facet Joint Syndrome: Treating arthritis or damage in the small joints of the spine.
- Spinal Infections or Tumors: Minimally invasive removal or biopsy.
The Procedure
- Preoperative Preparations:
- Imaging studies (MRI, CT scans) confirm the diagnosis and surgical plan.
- Preoperative evaluations assess patient fitness for surgery.
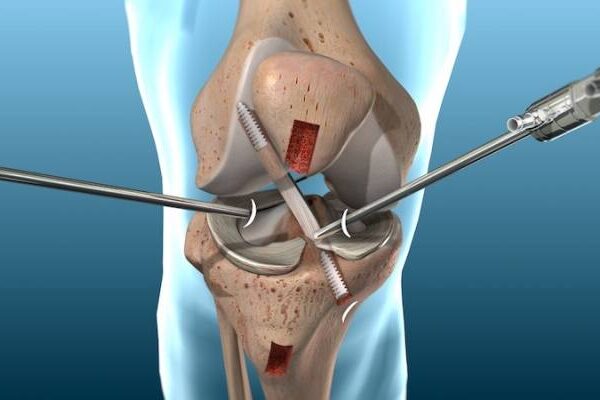
- During Surgery:
- Performed under local anesthesia with sedation or general anesthesia.
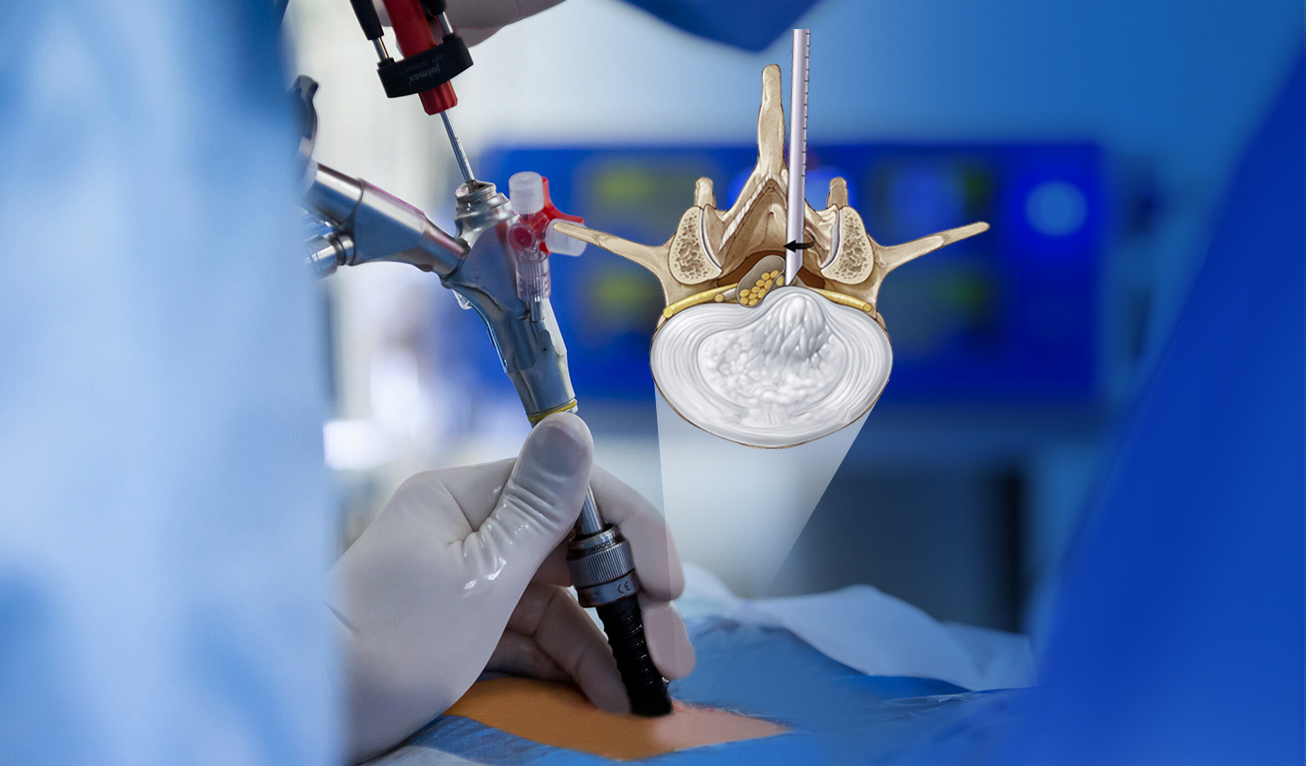
- A small incision (less than 1 cm) is made near the affected area.
- An endoscope, a thin tube with a camera and light, is inserted to visualize the spine.
- Specialized instruments are used to remove or repair damaged tissue while preserving surrounding structures.
- Continuous imaging (fluoroscopy) ensures precision during the procedure.
- Closure:
- The incision is closed with a few sutures or adhesive strips.
Recovery and Rehabilitation
- Immediate Postoperative Care:
- Most procedures are outpatient, allowing patients to go home the same day.
- Pain is typically mild and managed with medications.
- Walking and light activities are encouraged within hours post-surgery.
- Physical Therapy:
- May begin within a week to restore strength and flexibility.
- Focus on posture correction and core strengthening exercises.
- Return to Activities:
- Desk jobs: 1–2 weeks post-surgery.
- Physical labor or sports: 4–6 weeks, depending on the procedure and recovery.
Benefits of Endoscopic Spine Surgery
- Minimally Invasive:
- Small incisions and minimal tissue disruption.
- Reduced Pain:
- Faster pain relief compared to traditional surgery.
- Faster Recovery:
- Shorter rehabilitation periods.
- Low Risk of Complications:
- Lower infection and blood loss rates.
- Outpatient Procedure:
- Most patients go home the same day.
Risks and Complications
Although safer than open spine surgery, ESS carries potential risks such as:
- Infection at the surgical site.
- Nerve damage or persistent nerve pain.
- Incomplete symptom resolution.
- Rarely, the need for additional surgery.
Innovative Techniques in Endoscopic Spine Surgery
- Biportal Endoscopic Surgery:
- Uses two portals for improved visualization and access.
- Laser-Assisted Surgery:
- Laser technology for precision removal of damaged tissue.
- Robotic Assistance:
- Enhances accuracy in complex procedures.
- Navigational Systems:
- Real-time imaging for precise surgical guidance.
20 Questions & Answers on Endoscopic Spine Surgery
1. What is Endoscopic Spine Surgery?
A minimally invasive technique to treat spine conditions using a small endoscope and specialized instruments.
2. What conditions can ESS treat?
Herniated discs, spinal stenosis, sciatica, degenerative disc disease, and more.
3. How is ESS different from traditional spine surgery?
ESS uses small incisions, causes less tissue damage, and offers faster recovery.
4. What are the benefits of ESS?
Reduced pain, faster recovery, minimal scarring, and lower complication rates.
5. How long does ESS take?
Most procedures take 30 minutes to 2 hours, depending on the condition.
6. What type of anesthesia is used?
Local anesthesia with sedation or general anesthesia, depending on the procedure.
7. Can ESS be performed on an outpatient basis?
Yes, most ESS procedures are outpatient, allowing patients to go home the same day.
8. How soon can I walk after ESS?
Walking is typically encouraged within hours post-surgery.
9. How long does recovery take?
Recovery varies but generally ranges from 1–6 weeks.
10. Will I need physical therapy after ESS?
Yes, physical therapy helps restore strength, flexibility, and posture.
11. Are there risks associated with ESS?
Risks include infection, nerve damage, or incomplete symptom relief.
12. Is ESS effective for herniated discs?
Yes, it is one of the most common and successful procedures for this condition.
13. Can ESS treat sciatica?
Yes, by relieving pressure on the affected nerve.
14. Is ESS suitable for elderly patients?
Yes, its minimally invasive nature makes it ideal for older individuals with medical comorbidities.
15. How small are the incisions in ESS?
Incisions are typically less than 1 cm.
16. What imaging techniques are used during ESS?
Fluoroscopy or real-time imaging guides the procedure.
17. Can ESS address spinal stenosis?
Yes, it can decompress the spinal canal to alleviate symptoms.
18. Is ESS covered by insurance?
Most insurance plans cover ESS if deemed medically necessary.
19. What happens if symptoms persist after ESS?
A follow-up evaluation may determine if additional treatment is needed.
20. How do I prepare for ESS?
Follow preoperative instructions, such as fasting, stopping certain medications, and arranging transportation.